Bridging the Gap Series : March 2021
Introduction from Vice Chancellor Steve Goldstein
Access to fresh food, safe shelter and health services all support the wellbeing of communities—their absence in neighborhoods of color leads to health inequities. Over the last decade, pharmacies have closed in low-income neighborhoods and new ones have opened at more profitable locations. The COVID-19 pandemic has accelerated this trend. The straight line between pharmacy closures and dangerous health outcomes is well documented.
In this essay, part of the Bridging the Gap series where we focus on health equity, Cheryl Wisseh, health sciences assistant clinical professor, Department of Clinical Pharmacy Practice in the School of Pharmacy and Pharmaceutical Sciences at University of California, Irvine, discusses the growing problem of “pharmacy deserts” as a contributing cause for health inequity.
In her recent study, unique in its scope and design, Wisseh demonstrated that pharmacy deserts in the Los Angeles region are contributing to health inequity at an alarming rate in Black and Hispanic communities. She also uncovered a link between pharmacy deserts and generations of systemic racism and racial segregation in the residential regions of these communities.
The impact of pharmacies on health goes far beyond the critical provision of prescription medications in a safe manner. Pharmacists are an essential connection to the community delivering health guidance, which is particularly important in the management of chronic diseases and the facilitation of regimen maintenance, early detection of disease through health screening, and disease prevention through vaccine administration. Wisseh makes clear why we must confront the growing challenge of pharmacy deserts across the nation.
By Cheryl Wisseh, Assistant Clinical Professor, Department of Clinical Pharmacy Practice
At the University of California, Irvine, through research we recently uncovered a key indicator of racial inequality linked with health inequity in a seemingly unlikely place, but one which truly highlights how entrenched systematic racism is in our society. Pharmacy deserts, a lack of easy access to pharmacies, in the Los Angeles region are more likely to impact Black and Hispanic communities and this impacts health equity in a major way. The findings of our research harken back to a time when communities in LA were zoned by race. Pharmacy deserts align with a legacy of systemic racism and should be considered a major factor as we work towards eradicating health inequity and addressing issues of race in our communities.
Pharmacies play an essential role in our wellbeing and fulfill essential health care functions, such as health screenings, vaccines and medication management. They have been, and continue to be, essential during this COVID-19 pandemic helping to provide testing and also helping with vaccine rollout.
In the United States, and particularly in LA, a lack of access to nearby pharmacies has added to an already alarming rise in health disparities, especially amongst Black and Hispanic communities. This phenomenon, known as the pharmacy desert, got its name from an equally concerning trend, the food desert. Considering the racial inequities that the COVID-19 pandemic has laid bare, pharmacy deserts are an issue that our public health leaders ought to take to heart.
Historically, Black, Hispanic and low-income communities have had less access to local pharmacy services than non-Black, non-Hispanic communities. Our study, published in the Journal of Racial and Ethnic Health Disparities, is the first study to look at pharmacy deserts in the state of California and the LA region.
While this issue has been studied in the past, this new study focuses on pharmacy deserts within the context of social determinants health, not yet studied before in the Los Angeles region. These determinants are associated with socio-economic realities that have a direct impact on health and include factors such as access to personal mode of transportation such as vehicle ownership, and the rate of poverty and crime within a community. Our goal with this study was to examine the intersection between pharmacy, public health, and social justice in order to better address health disparities.
We found that pharmacies are closely linked to socio-economic situation and quality of healthcare. The study states, “As medications are commonly used to prevent and mitigate chronic diseases and their associated complications and outcomes, limited geographic access to medications in communities that are already plagued with health inequity is a growing concern. This is especially important because low-income urban minority communities often have high prevalence and incidence of cardiometabolic and respiratory chronic conditions.”
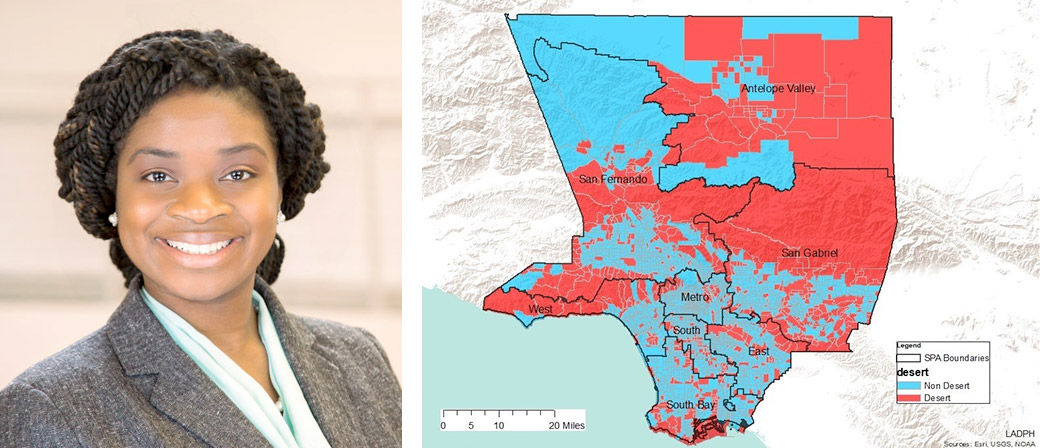
UCI has identified communities within Los Angeles where geographic pharmacy deserts exist. We used census tracts where the nearest community pharmacy was a mile or more away from the center what the study found was shocking. Not only was there a strong link between health disparities and pharmacy deserts, but more Black and Hispanic residents live in pharmacy deserts.
The findings show that LA Country pharmacy deserts are characterized by dense populations, a high numbers of renters and residents living under the federal poverty level, with more residents that speak English as a second language, less vehicle ownership, more Black and Hispanic residents, crime against property and people, and finally, less residents with health insurance, and fewer health professionals accessible to residents of the area. Residing in pharmacy desert areas not only belies equity issues due to significant levels of health disparities, but also adverse healthcare situations which are potentially compounded by the geographic shortage of pharmacies and pharmacy services.
What is possibly most concerning is that the LA County findings support the understanding of a historical evolution of pharmacy deserts in concert with structural inequity. Discriminatory practices such as racial zoning, which occurred prior to the civil rights era, had a hand in designating certain ethnicities to certain residential zones, generations later the impact is still felt by minority groups, specifically Black and Hispanic populations. Taking over from racial zoning, economic and cultural pressures have contributed disparities in areas prone to pharmacy deserts and health equity challenges which persist today.
The downward spiral effect that social economic factors have on health disparities and vice versa are especially troubling. If one can’t access basic health services provided by a pharmacy, they are more vulnerable to adverse health events and conditions which will present challenges to attending work or attaining an education both of which could contribute to being able to afford quality healthcare, and so the cycle continues.
We have much work ahead to break down structural and institutional strongholds which continue to enable racial inequity pharmacy deserts provide important markers. They represent areas where historic racial zoning maintains a dangerous impact on health and well-being, and a legacy of discrimination.
The findings of the study in LA County are appalling, but they can be used as a tool to improve healthcare for Black and Hispanic communities. Identifying pharmacy deserts indicates exactly where improved investments in pharmacy services must be made to increase access to healthcare in the long term, end harmful cycles and tear down these destructive systematic phenomena impacting Black and Hispanic communities.

Started in June 2020, Bridging the Gap is a series curated by Vice Chancellor Steve Goldstein, as a way to examine and share our work in closing all gaps to achieve health equity through awareness, understanding, compassion and action. You can also receive the series in your inbox by subscribing to the newsletter.
Category: Digital Publications